How must healthcare organization managers evaluate quality if they wish to be as effective as managers in non-healthcare industries?
They must do so
(1) in 'real time'
based on
(2) statistics (see above and below) and
(3) experiments (see below).
(Please consider using the subtitles provided while watching the YouTube video.)
Quality Management in Radiology
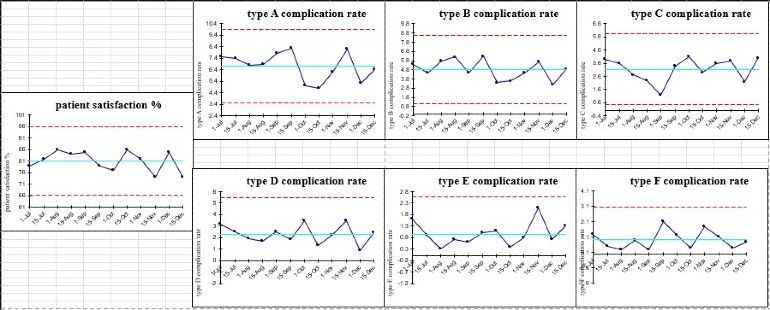
Below are examples of what I can do for your radiology department:
An effective manager makes decisions about what is best based on evidence, not expert opinion.
An opinion becomes expert when the opinion is highly familiar with the evidence.
Reliable evidence comes from 'experiments,' not 'experience' per se.
Exempli gratia:
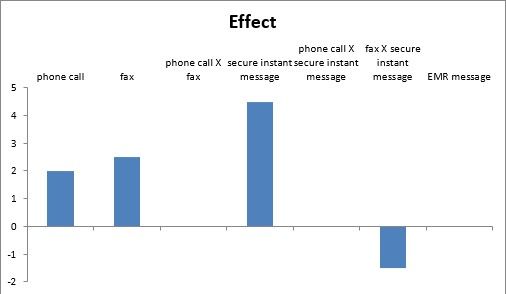
- A healthcare organization has too many errors and complaints regarding radiological report communication for incidental findings.
- Rather than relying on the chief medical officer's' 'authoritative opinion,' the quality manager conducted an experiment of four categorical factors divided into two levels using only ten experimental runs to show which option was the best, two runs each for five clinical departments.
- phone call... from a radiologist's assistant to a clinician's assistant vs. from radiologist to clinician
- text message via a HIPAA-compliant software... with vs. without a return acknowledgment of receipt
- fax... with vs. without a return acknowledgment of receipt
- EMR message... with vs. without a return acknowledgment of receipt
- The manager acquired quantitative feedback from (1) five clinical department chiefs and (2) the radiologist sending the communication regarding their satisfaction with the permutations of the different communication options.
Regarding this quasi-experiment:
- Can you interpret the confounding relationship between the phone call and EMR message factors?
- Can you tell whether an additional experiment needs to be performed to confirm the validity of this trial?
In general:
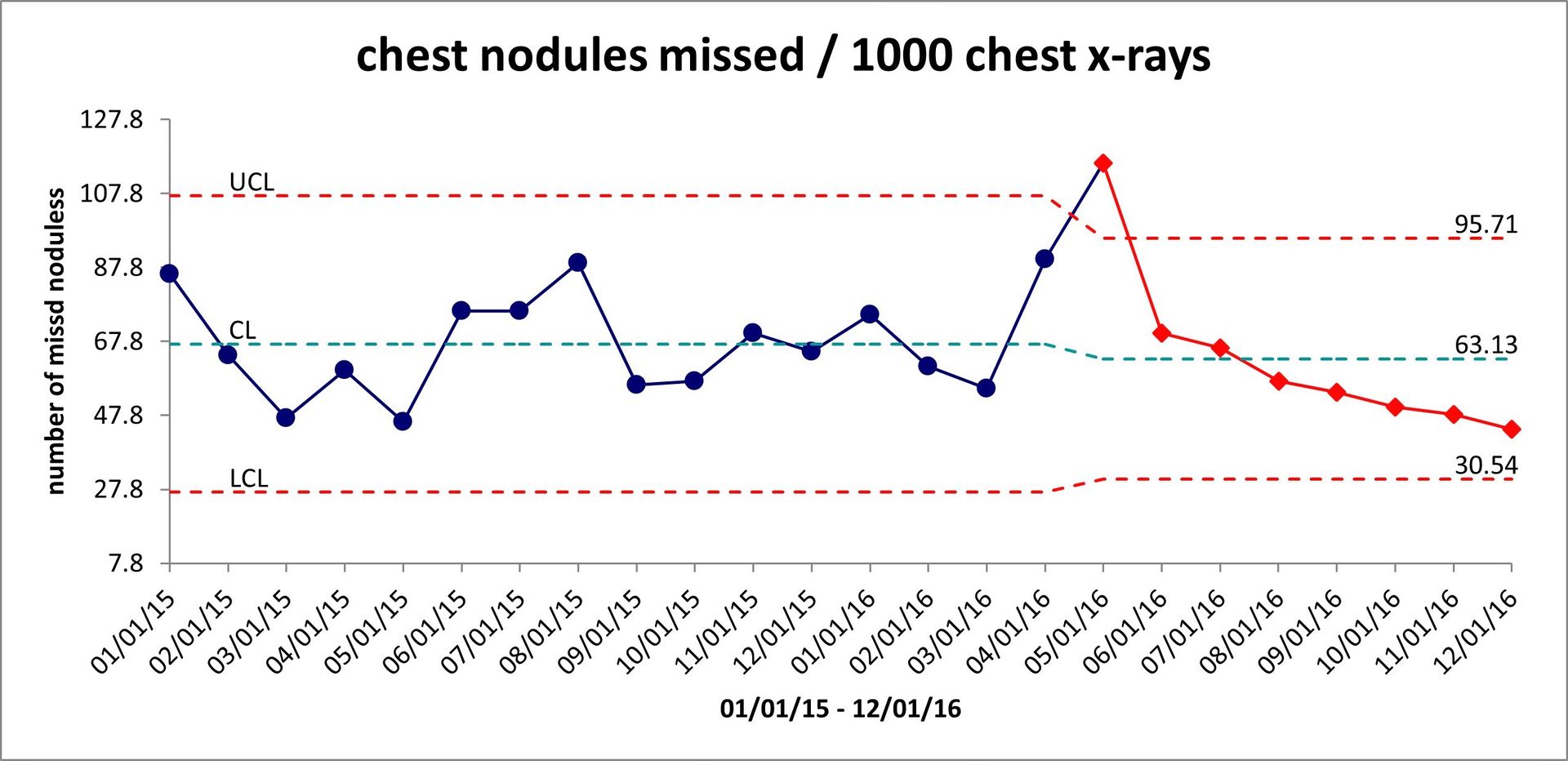
- Do you know (1) which math to use for control charts for the different data types (2) different ways to express a given set of data using control charts, and (3) how different distributions of data depend on factors (1) and (2) in order to make a control chart that will answer the clinical or business question you want to answer?
- Do you think a physician who knows how to implement evidence-based quality measures will add less value to your organization than one who can only generate RVUs?
If the answer to any of these questions is "No," then consider hiring a Certified Professional in Healthcare Quality.
assertions from
Peter Drucker
about managing
quality
"The purpose of business is to create and keep a customer."
The Practice of Management (1954), p. 37.
“Efficiency is concerned with doing things right. Effectiveness is doing the right things.”
“Unless we determine what shall be measured and what the yardstick of measurement in an area will be, the area itself will not be seen.”
What organization sets standards for healthcare professionals and non-healthcare professionals alike in managing healthcare quality?